Introduction to Creating a Baby Meal Plan (6-12 Months)
Designing a meal plan for babies aged 6 to 12 months is a crucial aspect of their development. This article explores the nutritional needs, safety guidelines, and meal suggestions to ensure your baby is getting the right balance of nutrients as they transition from breast milk or formula to solid foods.
Understanding Nutritional Needs
Understanding the nutritional needs of infants aged 6 to 12 months is crucial for their healthy development. During this period, babies experience rapid growth and development, which necessitates a careful balance of essential nutrients, vitamins, and minerals. Recognising these needs aids caregivers in formulating an effective meal plan that combines breast milk or formula with newly introduced solid foods.
From 6 to 12 months, the average infant needs approximately 750 to 900 calories per day. Around half of their caloric intake should come from breast milk or formula, as these remain vital sources of nutrients like protein and fats. Breast milk or formula should ideally make up 24 to 32 ounces daily, while the other half can be met through solid foods. It’s important to remember that each baby is different, and growth spurts often require adjustments to this caloric intake. Monitoring your baby’s signs of hunger and fullness will guide you in making the right adjustments.
One of the most critical nutrients for infants during this stage is iron. Iron is essential for cognitive development and the prevention of anaemia. At around 6 months, a baby’s natural iron stores begin to deplete, and introducing iron-rich foods becomes paramount. Good sources of iron include pureed meats, fortified cereals, and legumes. Pairing iron-rich foods with vitamin C sources, such as pureed fruits or vegetables, can enhance iron absorption.
In addition to iron, other vital nutrients that should be incorporated into an infant’s diet include calcium, which is essential for bone health; zinc, necessary for growth and immune function; and essential fatty acids, which support brain development. Dairy products, like yoghurt and cheese, provide calcium. Whole grains, nuts (if age-appropriate), and lean meats can supply zinc. Foods containing omega-3 fatty acids, such as fish and flaxseed, are beneficial as well.
As you introduce solid foods, it’s essential to diversify your baby’s diet. The first few months of solid food introduction should focus on single-grain cereals and pureed vegetables and fruits. Gradually introduce a variety of colours and textures, as this not only ensures a broad spectrum of nutrients but also exposes your baby to different flavours and helps them develop a preference for more diverse foods as they grow.
The frequency of meals is equally important. At 6 months, you can start with one to two meals of solid food per day. By the time they reach 9 months, it can be increased to two to three meals, supplemented with healthy snacks. It’s crucial to establish a routine. Feeding your baby at the same time every day can help them regulate hunger signals. As they approach 12 months, most babies will be eating three meals a day, with snacks in between. Caregivers should remain flexible, making adjustments based on the baby’s appetite, preferences, and developmental milestones.
As you build your baby’s meal plan, always be attentive to their developmental readiness for more complex foods. This might involve introducing soft finger foods or moving toward mashable textures as they master chewing. Keeping an eye on the developmental milestones can ensure that your baby is prepared for these advances in their diet.
It’s also important to remain aware that while breast milk or formula continues to be significant, solid foods should not be offered at the expense of these primary sources of nutrition during the first year. A balance is key. For instance, if a baby is consuming a significant volume of solids, ensure it does not result in a decreased intake of milk or formula. The timing can also play a role; offering solids after a milk feeding can help ensure they are getting adequate nutrition from both sources.
Overall, creating a nutritious meal plan for infants aged 6 to 12 months requires attention to their evolving nutritional needs. Emphasising iron and incorporating an array of food choices can help establish healthy eating habits early. By offering a balance of breast milk or formula along with solid foods and adjusting feeding frequencies as needed, caregivers can foster a positive feeding experience that supports optimal growth and development. Keeping these guidelines in mind will lay the groundwork not only for a balanced diet during infancy but for a lifetime of healthy eating practices.
Safe and Simple Food Allergy Prevention
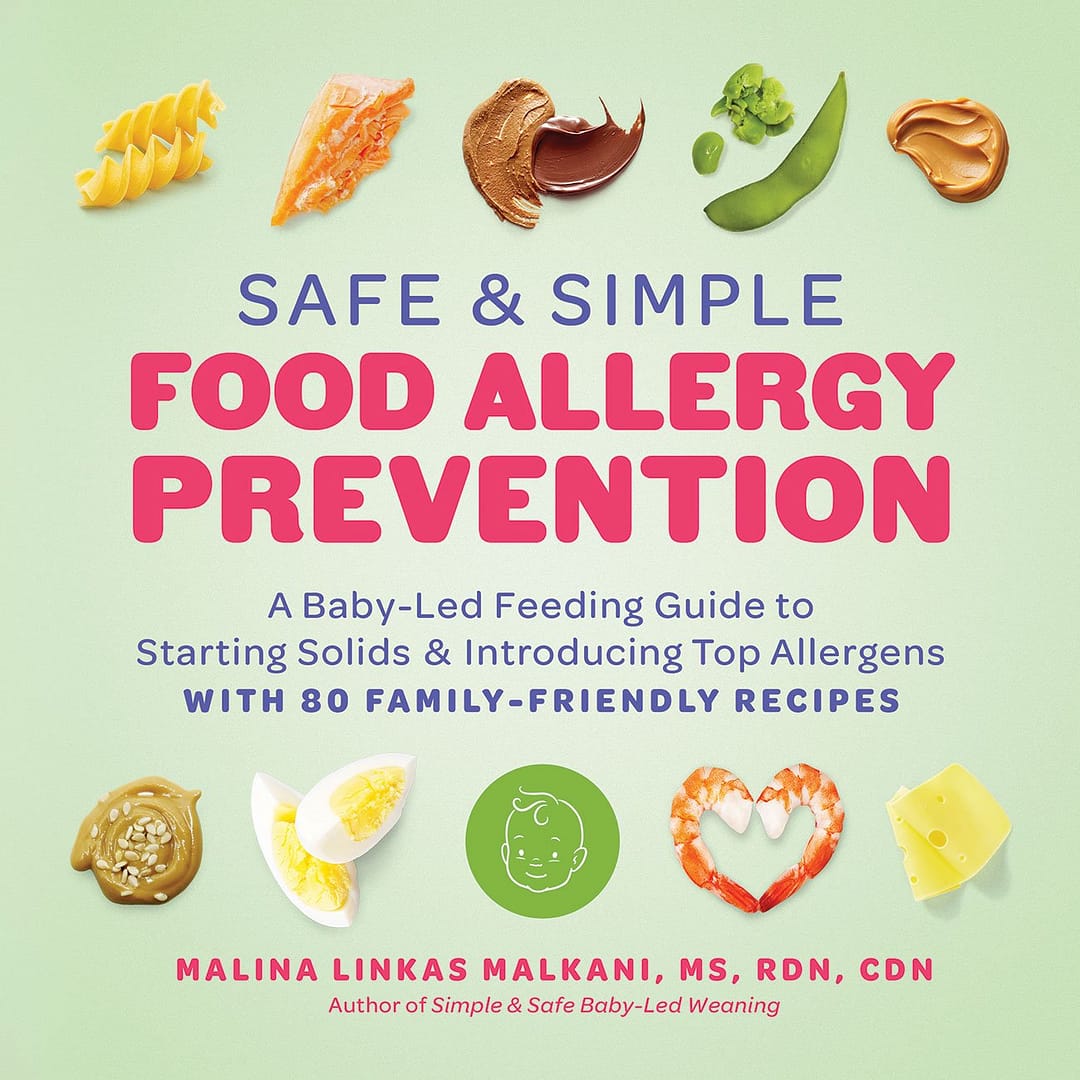
Disclosure: As an Amazon Associate, I earn from qualifying purchases. This means that if you click on a link and make a purchase, I may receive a small commission at no additional cost to you.
Safety Guidelines for Introducing Solids
As you embark on the journey of introducing solid foods to your baby, safety is of utmost importance. When planning meals for infants aged 6 to 12 months, several critical safety measures must be taken into consideration to ensure their health and well-being. Understanding food allergies, choking hazards, and the concept of introducing one new food at a time plays a fundamental role in creating a safe eating environment for your little one.
First and foremost, be vigilant about food allergies. Food allergy reactions in infants can range from mild to severe, making it essential to introduce potentially allergenic foods with care. Common allergens include dairy, eggs, peanuts, tree nuts, fish, shellfish, soy, and wheat. To minimise the risk of an allergic reaction, it is advised to introduce these foods one at a time while monitoring your baby’s reaction over the course of three to five days. Observing your baby for signs such as hives, swelling, vomiting, or breathing difficulties after a new food is introduced is crucial. If any concerning symptoms arise, consult a paediatrician immediately.
It is also imperative to be aware of choking hazards. Babies at this stage are typically beginning to develop their ability to chew; however, their gag reflex may still be quite strong, and their swallowing skills are not yet fully developed. To prevent choking incidents, foods should be prepared in appropriate sizes and textures. Soft foods should be mashed or pureed, while finger foods should be cut into small, manageable pieces that are easy for your baby to grasp. Foods that are usually considered choking hazards, such as whole grapes, nuts, popcorn, raw vegetables, and chunks of meat, should not be given to infants. Instead, soften or modify textures to an appropriate consistency, ensuring that meals are safe for your baby to explore.
Recognising readiness signs is another guideline worth emphasising when introducing solids. Not all infants are ready for solid foods at the same time, even if they fall within the 6 to 12-month age range. Some physical signs that indicate your baby may be ready for solids include the ability to sit up independently, showing interest in the food others are eating, and the ability to move food to the back of their mouth to swallow. Watch for these cues, as they suggest your child is physically and developmentally prepared to start this new phase of eating.
Moreover, while it’s exciting to introduce your baby to a variety of new tastes and textures, doing so incrementally is essential. Implementing the practice of introducing one new food at a time allows you to accurately track how your baby responds to each new introduction. This strategy not only identifies potential food allergies or intolerances more clearly but also eases the transition for your baby into the world of solid foods. Starting with single-grain cereals or pureed fruits and vegetables can be a gentle introduction, gradually progressing to more complex combinations as your baby grows comfortable.
Patience and attentiveness are key during this time. Each new food experience is an opportunity to learn about your baby’s preferences and aversions. Monitoring their reactions and understanding their cues will help you discern whether they are ready for new foods or require more time with those already introduced. Additionally, the developmental phase during which your baby explores solid foods may sometimes involve interesting reactions, including expressions of distaste or refusal. These responses are normal and part of your baby’s development in discovering their unique tastes.
Incorporating safety guidelines into your meal planning process means prioritising your baby’s health while fostering a positive mealtime experience. Always wash your hands and prepare food in a clean environment to reduce the risk of foodborne illness. Educating yourself about appropriate food handling and storage practices adds another layer of safety. Make sure to refrigerate leftovers promptly, and keep perishable foods out of the “danger zone” of temperatures that promote bacterial growth.
Moreover, consider keeping emergency contacts, such as your paediatrician or a local expert, on hand for any urgent queries regarding food-related concerns. Building a robust knowledge base about food introduction will give you confidence in navigating this intricate stage of feeding.
As you refine your baby meal plan, considering these safety measures, remember that this stage is filled with exploration and discovery. Your careful planning and attention to safety will ensure that mealtimes nurture not only your baby’s growth but also their confidence in the world of food. Creating a secure and enjoyable eating environment sets the foundation for developing healthy eating habits as they grow.
Top 100 Baby Purees
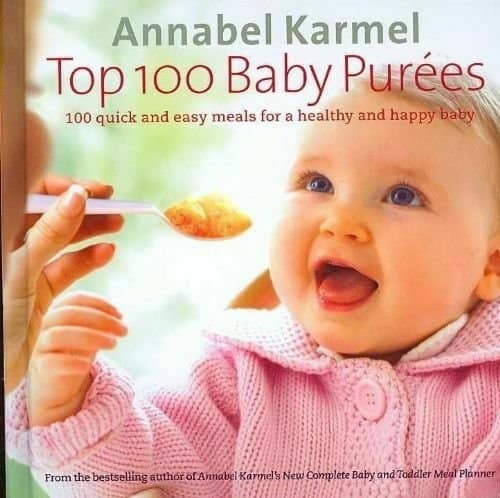
Disclosure: As an Amazon Associate, I earn from qualifying purchases. This means that if you click on a link and make a purchase, I may receive a small commission at no additional cost to you.
Creating a Balanced Meal Plan
Creating a balanced meal plan for your baby between 6 to 12 months is essential for ensuring they receive the necessary nutrients for their growth and development. At this stage, babies are transitioning from breast milk or formula to solid foods, and a well-structured meal plan can help introduce a variety of flavours and textures while also meeting their evolving dietary needs. It’s important to incorporate a range of food groups, including fruits, vegetables, grains, proteins, and dairy, to create a diverse and enjoyable culinary experience for your baby.
When developing a weekly meal plan, the first step is to establish a routine. Babies thrive on consistency, so offering meals and snacks at the same times each day can help them feel secure and understand when it’s time to eat. A sample daily structure could include three meals and two snacks. Below is an example of a balanced meal plan for a week:
Day 1:
– Breakfast: Oatmeal made with breast milk or formula (4-6 tbsp) mixed with pureed apples (2 tbsp).
– Lunch: Mashed avocado (2-3 tbsp) with soft-cooked quinoa (2-4 tbsp).
– Snack: Steamed carrot sticks or cucumber sticks (1-2 pieces).
– Dinner: Pureed sweet potato (4 tbsp) with shredded chicken (2 tbsp).
Day 2:
– Breakfast: Banana pancakes (1 small pancake) made from mashed banana and egg.
– Lunch: Pureed peas (4 tbsp) with mashed potatoes (4 tbsp).
– Snack: Soft toast strips (1 slice) with a thin spread of unsweetened apple butter.
– Dinner: Turkey puree (2-4 tbsp) with soft-cooked brown rice (2 tbsp).
Day 3:
– Breakfast: Yoghurt (unsweetened, full-fat) (2-4 tbsp) mixed with a small amount of pureed peaches.
– Lunch: Pasta (well-cooked, cut into small pieces) (2-4 tbsp) with pureed spinach (2 tbsp).
– Snack: Sliced ripe pear (2 slices) or a thin slice of soft cheese.
– Dinner: Mashed butternut squash (4 tbsp) with lentils (2 tbsp).
Day 4:
– Breakfast: Rice cereal (4 tbsp) mixed with pear puree (2 tbsp).
– Lunch: Pureed carrot and green bean mix (2-4 tbsp).
– Snack: Mashed blueberries (2 tbsp) on oatmeal or soft rice cakes.
– Dinner: Ground turkey (2-4 tbsp) with small pieces of steamed broccoli.
Day 5:
– Breakfast: Whole grain toast fingers (1 slice) with thinly spread peanut butter (check for allergies).
– Lunch: Creamed corn (pureed) (2-4 tbsp) with soft potato cubes.
– Snack: Soft fruit slices (such as banana or kiwi).
– Dinner: Pureed chickpeas (2-4 tbsp) with mashed cauliflower (4 tbsp).
Day 6:
– Breakfast: Quinoa breakfast porridge (2-4 tbsp) topped with mashed avocado.
– Lunch: Roasted sweet potato cubes (2-4 tbsp) with finely shredded chicken (2 tbsp).
– Snack: Soft-cooked broccoli florets (2-3 pieces).
– Dinner: Pureed beetroot (4 tbsp) with small pieces of soft-cooked fish (2 tbsp).
Day 7:
– Breakfast: Smoothie with yoghurt (2-4 tbsp) blended with banana and a touch of spinach.
– Lunch: Zucchini fritters (1-2 small) made with finely grated zucchini and egg.
– Snack: Fresh fruit puree (such as mango) (2 tbsp) or small morsels of soft-cooked pasta.
– Dinner: Natural yoghurt (2-4 tbsp) with pureed fruit mixed in.
Portion sizes will differ based on your baby’s age, appetite, and developmental stage. Starting with smaller amounts and gradually increasing as your baby becomes comfortable with eating solid foods is key. Monitor them closely; they may eat more or less on different days, depending on their hunger levels or growth spurts.
Preparing food at home is beneficial in multiple ways. Not only do you control the ingredients, but you can also tailor flavours and textures to your baby’s preferences. Start with smooth purees and gradually introduce lumpier textures as your baby becomes accustomed to chewing. You can make purees using fresh or frozen fruits and vegetables, which should qualify as the main components of your baby’s meals. For proteins, think about cooking methods like poaching or steaming to keep food tender and safe.
When introducing new foods, remember to incorporate one new ingredient at a time every few days. This strategy helps monitor for any potential allergic reactions. Additionally, offering a combination of colours and textures can make meals visually appealing and more enticing for your baby.
As you build your weekly meal plan, remain patient and flexible. Babies may have varying tastes each day, so be ready to substitute ingredients or try new combinations if something doesn’t work out. The journey of introducing solid foods should be enjoyable for both you and your baby, encouraging exploration and forming healthy eating habits that will last a lifetime.
Addressing Common Challenges and Concerns
As you embark on the journey of introducing solid foods to your baby, it’s crucial to address common challenges that may arise during this phase. Many parents may experience concerns such as food rejection, constipation, and the overall stress associated with mealtimes. Understanding these challenges and knowing how to tackle them will not only make the process smoother for you and your baby but also foster positive eating habits that can last a lifetime.
One of the most frequent issues parents face is food rejection. It’s entirely normal for babies to turn their noses up at new foods. Their taste buds are still developing, and they may be wary of unfamiliar flavours and textures. If your little one refuses a certain food, try not to take it personally. Instead, consider offering the same food again after a few days or even weeks. Research indicates that it can take multiple exposures, sometimes as many as 10 to 15 times, before a baby accepts a new food. You can also try providing the food in various forms; for example, if your baby rejects pureed carrots, you might try baked carrot sticks or steamed carrot rounds. The key is persistence and variety.
To encourage a positive eating experience, make mealtimes engaging and fun. Create an inviting atmosphere by sitting together as a family during meals. This not only provides a model for healthy eating but also sets the stage for social interaction. Allow your baby to explore foods with their hands, if appropriate. Messy play can help familiarise them with different textures and tastes, easing fears about new foods. Remember, your reactions matter too; if you show enthusiasm and curiosity about the foods being served, your baby is more likely to mimic that excitement.
Another concern many parents encounter is constipation, which can be a common side effect as babies transition to solid foods. As your baby begins to eat a greater variety of foods, they may consume less breast milk or formula, which can lead to firmer stools. To help alleviate constipation, prioritise fibre-rich foods such as pureed or mashed fruits (like prunes and pears) and vegetables (like peas and sweet potatoes) in your meal plan. Whole grains, such as oatmeal or brown rice, can also aid in maintaining digestive health. Ensuring your baby remains well-hydrated is essential too; offering small sips of water with meals can help soften stools.
If constipation persists, make adjustments in your food choices gradually and observe how your baby responds. It can be useful to maintain a food diary so you can track which foods are well accepted and which may be causing digestive issues. Additionally, incorporating physical activity, like tummy time and rolling, can promote digestion and help keep things moving.
Be aware that some babies may experience allergic reactions to certain foods. Always introduce new foods one at a time, and wait a few days before trying another new item. This way, if your baby has a reaction, you can identify the source more easily. Common allergenic foods include dairy, nuts, eggs, and shellfish, so it is essential to approach these with care, especially if there’s a family history of allergies.
To reduce stress around feeding, establish a consistent routine. Offering meals and snacks at roughly the same times each day provides a sense of security and predictability for your baby. When preparing meals, keep them simple and allow them to evolve over time. You might start with purees and gradually introduce soft chunks before moving to more textured foods. Giving your baby some control over their eating by allowing them to pick from a selection of foods can also encourage more independent eating habits.
Support from healthcare professionals can be incredibly valuable. Don’t hesitate to reach out to your paediatrician or a registered dietitian if you have concerns about your baby’s eating habits or growth patterns. They can provide tailored advice that considers your baby’s individual needs as well as any underlying health factors.
Lastly, remember that the goal at this stage is not perfection but rather to cultivate a positive association with food. Patience is key, and remaining calm and flexible will help you tackle any obstacles you may encounter. By addressing common challenges compassionately and effectively, you’ll create a nurturing feeding environment that supports your baby’s development and sets the groundwork for a lifelong relationship with healthy eating.
Conclusion
In conclusion, a well-structured meal plan for infants aged 6 to 12 months is vital for their health and development. By incorporating a variety of foods, adhering to safety guidelines, and ensuring proper nutritional intake, you can foster a positive relationship with food and support your baby’s growth effectively.
Frequently Asked Questions – Creating a Baby Meal Plan
When should I start introducing solid foods to my baby?
You can start introducing solid foods around 6 months of age when your baby shows signs of readiness. Look for physical signs like the ability to sit up independently, showing interest in the food others are eating, and the ability to move food to the back of their mouth to swallow. Not all babies are ready at exactly 6 months, so watch for these developmental cues.
How much should my baby eat each day?
Babies aged 6-12 months need approximately 750-900 calories per day. About half of their caloric intake should still come from breast milk or formula (24-32 ounces daily), while the other half comes from solid foods. Start with smaller portions and gradually increase as your baby becomes comfortable with eating solids. Remember that each baby is different, and their appetite may vary day to day.
What are the most important nutrients for my baby at this stage?
Iron is one of the most critical nutrients since babies’ natural iron stores begin to deplete around 6 months. Include iron-rich foods like pureed meats, fortified cereals, and legumes. Other essential nutrients include calcium for bone health, zinc for growth and immune function, and omega-3 fatty acids for brain development. Pair iron-rich foods with vitamin C sources to enhance absorption.
How do I safely introduce potentially allergenic foods?
Introduce potentially allergenic foods one at a time and monitor your baby’s reaction for 3-5 days before introducing another new food. Common allergens include dairy, eggs, peanuts, tree nuts, fish, shellfish, soy, and wheat. Watch for signs like hives, swelling, vomiting, or breathing difficulties. If any concerning symptoms arise, consult your paediatrician immediately.
What should I do if my baby keeps rejecting certain foods?
Food rejection is completely normal and part of your baby’s development. It can take 10-15 exposures before a baby accepts a new food, so be patient and persistent. Try offering the same food in different forms or preparations. Make mealtimes engaging by eating together as a family and allowing your baby to explore foods with their hands when appropriate.
How can I prevent choking hazards?
Prepare foods in appropriate sizes and textures for your baby’s developmental stage. Soft foods should be mashed or pureed, while finger foods should be cut into small, manageable pieces. Avoid whole grapes, nuts, popcorn, raw vegetables, and chunks of meat. As your baby develops better chewing skills, you can gradually introduce more textured foods.
What should I do if my baby becomes constipated after starting solids?
Constipation is common as babies transition to solid foods. Include fibre-rich foods like pureed fruits (prunes and pears) and vegetables (peas and sweet potatoes) in your meal plan. Whole grains like oatmeal or brown rice can also help. Ensure your baby stays well-hydrated by offering small sips of water with meals. If constipation persists, consult your paediatrician for personalised advice.
Further Reading
- Exploring Baby-Led Weaning and Traditional Spoon-Feeding
- Baby Food Allergies: Symptoms and Prevention
- Introducing Solid Foods: A Month-by-Month Guide
- Baby Milestones: What to Expect in the 1st Year
PewinGo Weaning Bib

- Image for illustration only – Designs vary
Disclosure: As an Amazon Associate, I earn from qualifying purchases. This means that if you click on a link and make a purchase, I may receive a small commission at no additional cost to you.
Creating a Baby Meal Plan (6-12 Months) Podcast
As the podcast is hosted on Spotify, you may need to refresh the page to pull in the podcast.
References and Sources
NHS Official Resources
- What to feed your baby (10-12 months): https://www.nhs.uk/start-for-life/baby/weaning/what-to-feed-your-baby/10-to-12-months/
- What to feed over 12 months: https://www.nhs.uk/start-for-life/baby/weaning/what-to-feed-your-baby/over-12-months/
- Your baby’s first solid foods: https://www.nhs.uk/baby/weaning-and-feeding/babys-first-solid-foods/
Government Health Departments
- New campaign on introducing solid foods: https://www.gov.uk/government/news/new-campaign-promotes-advice-to-introduce-babies-to-solid-food
- SACN Report on feeding young children (1-5 years): https://www.gov.uk/government/publications/sacn-report-feeding-young-children-aged-1-to-5-years/feeding-young-children-aged-1-to-5-years-summary-report
- Early Years Foundation Stage nutrition guidance: https://www.gov.uk/government/publications/early-years-foundation-stage-nutrition
Professional Health Organisations
UNICEF UK Baby Friendly Initiative
Start4Life Introducing Solid Foods guide: https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2008/02/Start4Life-Introducing-Solid-Foods-2015.pdf
The Caroline Walker Trust
Eating well in the first year of life: https://www.cwt.org.uk/wp-content/uploads/2014/07/CHEW-1stYearLifePracticalGuide.pdf